Introduction: Eye Inflammation and Migraines
As someone who has experienced migraines and eye inflammation, I've often wondered if there might be a connection between the two. In this article, we will explore the possible link between eye inflammation and migraines, discussing the different types of eye inflammation, the causes of migraines, and how the two may be related. We will also look at some potential triggers for these conditions, as well as ways to manage and prevent them.
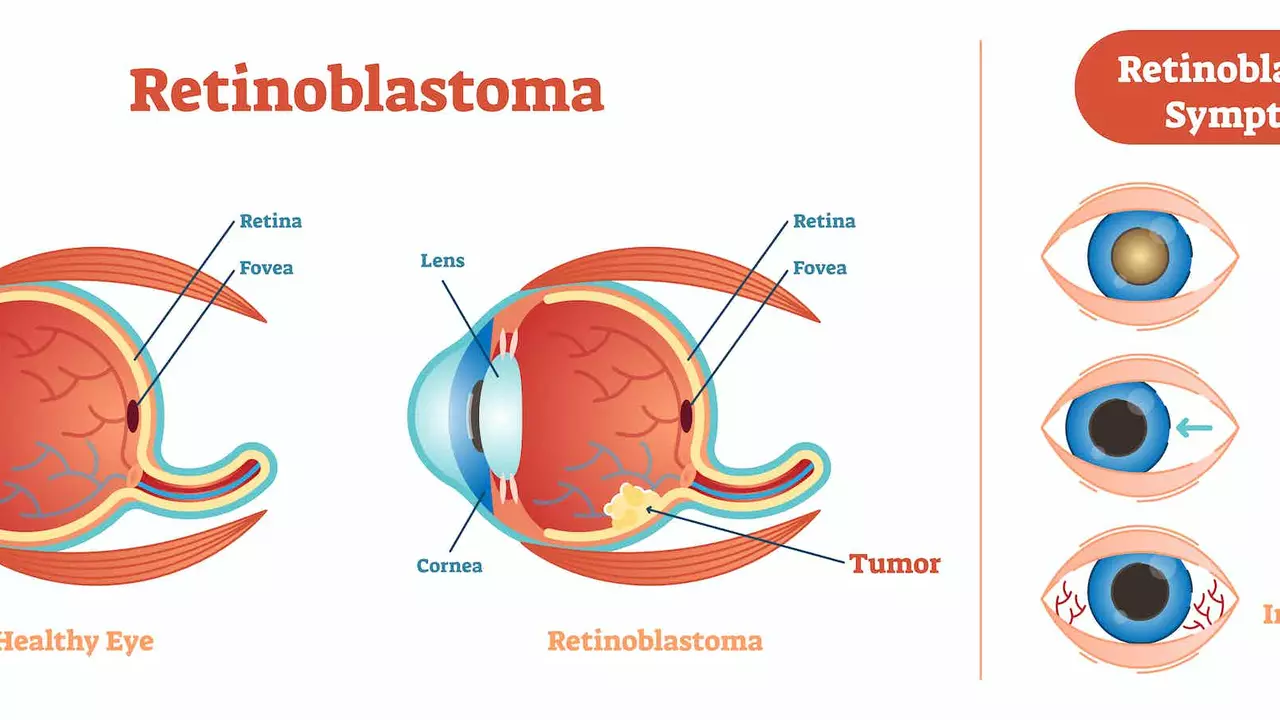
Types of Eye Inflammation
Eye inflammation can come in many forms, and it's important to understand the different types in order to better understand any potential connections with migraines. Some common types of eye inflammation include:
Conjunctivitis
Also known as "pink eye," conjunctivitis is an inflammation of the conjunctiva, the thin layer that covers the white part of the eye and the inside of the eyelids. It can be caused by allergies, bacteria, or viruses, and is characterized by redness, itching, and discharge.
Uveitis
Uveitis is an inflammation of the uvea, which is the middle layer of the eye that contains blood vessels. This condition can be caused by an autoimmune disorder, infection, or injury, and can lead to blurred vision, pain, and sensitivity to light.
Blepharitis
Blepharitis is an inflammation of the eyelids, typically caused by a bacterial infection or a skin condition like rosacea or seborrheic dermatitis. Symptoms can include itching, redness, and crusting along the eyelash line.
Understanding Migraines
Migraines are a type of headache that can cause severe pain, often accompanied by other symptoms like nausea, vomiting, and sensitivity to light and sound. Migraines are believed to be caused by a combination of genetic and environmental factors, and can be triggered by various factors such as hormonal changes, stress, certain foods or beverages, and changes in sleep patterns.
There are two main types of migraines: those with aura and those without. Auras are visual disturbances that can occur before or during a migraine, and may include seeing flashing lights, zigzag lines, or blind spots. Not everyone who experiences migraines will have auras, but for those who do, they can be a warning sign that a migraine is on its way.
The Connection Between Eye Inflammation and Migraines
While there is no definitive answer to whether eye inflammation and migraines are directly connected, there are some potential links that have been explored in research. One theory is that inflammation in the eye can trigger the release of certain chemicals, which can then cause blood vessels in the brain to constrict and lead to a migraine.
Another possible connection is that both eye inflammation and migraines can be triggered by similar factors, such as allergies, stress, and lack of sleep. This could mean that people who are prone to one condition may also be more likely to experience the other.
Triggers for Eye Inflammation and Migraines
As mentioned earlier, both eye inflammation and migraines can be triggered by a variety of factors. Some common triggers for eye inflammation include:
- Allergies
- Exposure to irritants, such as smoke or chemicals
- Eye injuries
- Infections
Common migraine triggers include:
- Stress
- Hormonal changes, such as those experienced during menstruation
- Certain foods and beverages, like chocolate, caffeine, and alcohol
- Changes in sleep patterns or lack of sleep
Managing and Preventing Eye Inflammation and Migraines
While there may not be a direct connection between eye inflammation and migraines, there are still steps that can be taken to manage and prevent both conditions. For eye inflammation, this may include:
- Using over-the-counter eye drops or prescription medications, as recommended by a healthcare professional
- Avoiding allergens and irritants, and using allergy medications as needed
- Practicing good eye hygiene, such as washing your hands before touching your eyes and removing makeup before bed
For migraines, management and prevention strategies may involve:
- Identifying and avoiding personal triggers
- Taking over-the-counter or prescription medications as directed by a healthcare professional
- Maintaining a regular sleep schedule and practicing good sleep hygiene
- Managing stress through relaxation techniques, exercise, or therapy
When to See a Healthcare Professional
If you're experiencing frequent or severe eye inflammation or migraines, it's important to consult with a healthcare professional. They can help determine the underlying cause of your symptoms and recommend appropriate treatment options. Additionally, if you're concerned about a possible connection between your eye inflammation and migraines, discussing this with your healthcare provider can help provide further insight and guidance.
Conclusion: Eye Inflammation and Migraines
While there may not be a direct connection between eye inflammation and migraines, it's clear that both conditions can have a significant impact on a person's quality of life. By understanding the potential triggers and management strategies for both conditions, it's possible to minimize their impact and improve overall well-being. Remember, it's always important to consult with a healthcare professional if you're concerned about your symptoms or need guidance on managing these conditions.





Shan Reddy
Hey everyone, I’ve found that keeping a simple eye‑care routine really helps when the eyes feel itchy or red. Regularly using preservative‑free drops and taking short breaks from screens can cut down on irritation. Also, staying hydrated and getting enough sleep often eases both eye inflammation and migraine frequency. Hope this helps!
CASEY PERRY
The pathophysiological overlap implicates neuroinflammatory mediators, yet causality remains unsubstantiated.
Naomi Shimberg
While the article posits a plausible link, it neglects the extensive literature demonstrating independent etiology for ocular inflammation. One must consider that attributing migraine exacerbation to peripheral ocular factors may oversimplify a complex neurovascular phenomenon. Consequently, the purported connection appears tenuous at best.
kenny lastimosa
It is interesting to ponder whether the eye, as a sensory portal, merely reflects systemic disturbances or actively participates in them. Perhaps the inflammation serves as a peripheral signal, triggering central sensitization that culminates in a migraine. Such musings remind us that bodily systems rarely operate in isolation.
Heather ehlschide
From a clinical standpoint, it is essential to differentiate the type of ocular inflammation before selecting a treatment plan. For conjunctivitis, antihistamine or antibiotic eye drops are often effective, whereas uveitis typically requires steroidal therapy under ophthalmologic supervision. Moreover, patients should track migraine triggers alongside eye symptoms to identify any patterns. Implementing a symptom diary can be a valuable tool in this process.
Kajal Gupta
Honestly, dealing with pink eye and thundering head‑aches at the same time feels like a double‑whammy of misery, but don’t let it get you down! Try swapping out harsh soaps for gentle, hypo‑allergenic cleansers, and keep a stash of cool compresses handy for that burning sensation. And remember, a pinch of humor and a dash of patience go a long way on the road to recovery.
Zachary Blackwell
Just so you know, the pharma industry doesn’t want you to connect the dots between eye inflammation and migraines because it would push them to develop a combined therapy that could cut their profit margins. Keep your eyes peeled-literally-and consider natural anti‑inflammatory foods like turmeric and omega‑3s to stay ahead of the game.
prithi mallick
Hey love, i totally get how overwhelming it can be when both your eyes and head feel like they’re on fire. try to give yourself some gentle breaks, like closing your lids for a minute every hour and sipping warm water. also, a little meditation can calm the stress that might be fueling both issues. you got this!
Michaela Dixon
Eye inflammation can be a tricky beast because it shows up in many forms and each form can have its own set of triggers. Some people notice that when the pollen count spikes their eyes start to itch and get red, and that same allergic response can set off a migraine later in the day. Others report that a cold sore near the eye can cause irritation and then a pounding headache that feels like a migraine. The brain and the eye share many of the same blood vessels and nerve pathways, so it is not surprising that a problem in one area can echo in the other. Inflammation releases chemicals like cytokines that can travel through the bloodstream and affect the nervous system. Those chemicals can cause blood vessels in the brain to constrict or dilate, which is a classic trigger for migraine pain. At the same time, the eyes are very sensitive to light, and bright light is a well‑known migraine trigger. This double hit of sensitivity can worsen the situation quickly. Lifestyle factors such as poor sleep, stress, and dehydration can fuel both eye inflammation and migraines simultaneously. Adding to the mix, certain foods that cause histamine release can brighten both the eyes and the headache. Some studies have even suggested that treating the eye inflammation aggressively can reduce the frequency of migraine attacks. However, the evidence is still emerging and more research is needed to draw firm conclusions. If you are dealing with both conditions it may be helpful to keep a detailed diary of symptoms and possible triggers. Seeing a specialist who understands both ophthalmology and neurology can provide a more coordinated treatment plan. Ultimately, paying attention to your body’s warning signs and making small adjustments can go a long way toward breaking the cycle.
Dan Danuts
Great rundown! Just remember to stay positive, keep a regular schedule, and you’ll see improvements fast.
Dante Russello
When considering the overlap between ocular inflammation and migraine episodes, it is prudent to evaluate environmental allergens, dietary triggers, and stress levels, all of which can contribute to both conditions, and by doing so, patients may uncover common pathways that can be addressed with comprehensive lifestyle modifications.
James Gray
Yo, this is super helpful, thanks a lot!
Scott Ring
I hear you, dealing with eye irritation and migraines at the same time can feel exhausting, but taking small steps like eye‑hygiene routines and consistent sleep patterns often makes a noticeable difference over time.
Shubhi Sahni
Adding to Heather’s points, it is also useful to schedule regular follow‑ups with both an ophthalmologist and a neurologist, to ensure that any changes in symptom patterns are promptly evaluated, and to adjust treatment plans accordingly, which can greatly enhance overall management success.