When pancreatic cancer shows up, it’s often already far along. That’s why so many people hear the diagnosis too late. The pancreas sits deep behind the stomach, quiet and hidden, and when something goes wrong there, the body doesn’t scream-it whispers. By the time the signs are clear enough to act on, the cancer may have spread. But things are changing. New research is uncovering earlier warning signs, and treatments that once seemed hopeless are now giving people more time, sometimes even a chance at recovery.
What Are the Early Signs You Might Be Missing?
- Unexplained weight loss-you’re eating normally, maybe even more than usual, but the scale keeps dropping. This happens in about 60% of cases, often before any other symptoms show up.
- Abdominal or back pain-not the kind from eating too much or a pulled muscle. This pain is dull, constant, and gets worse after eating or when lying down. It’s reported in 65-75% of patients.
- Jaundice-yellow skin or eyes, dark urine, and pale, greasy stools. This happens when a tumor in the head of the pancreas blocks the bile duct. About 70% of patients with tumors in that area develop jaundice, and 60% of them also feel intense itching.
- New-onset diabetes-if you’ve never had diabetes before and suddenly your blood sugar spikes, especially after age 50, it could be a red flag. Research shows 80% of pancreatic cancer patients develop diabetes within 18 months of their diagnosis. Fasting glucose levels jump from normal (under 100 mg/dL) to diabetic levels (over 126 mg/dL) in just a few months.
- Loss of appetite and nausea-you lose interest in food, feel full fast, or get sick after eating. These aren’t just "off days." They’re persistent, and they don’t go away with rest or changes in diet.
- Depression or anxiety that comes out of nowhere-this one surprises many people. A 2018 study found that over a third of patients had major mood changes before any physical symptoms. For half of them, depression was the first clue something was wrong.
These symptoms don’t mean you have pancreatic cancer. They’re common in many other conditions-gallstones, IBS, stress, even aging. But if you’re experiencing two or more of them together, especially if you’re over 50 or have a family history of cancer, don’t brush them off. Talk to your doctor. Early detection can make all the difference.
Why Is Pancreatic Cancer So Hard to Catch Early?
The pancreas is tucked behind the stomach, out of reach for regular exams. You can’t feel a tumor there by pressing on your belly. There’s no simple blood test or scan that works for everyone. The most common blood marker, CA 19-9, only shows up in advanced cases. Even CT scans miss tumors smaller than 2 cm about 40% of the time.
That’s why screening isn’t recommended for the general public. But for people at high risk-those with BRCA gene mutations, hereditary pancreatitis, or a strong family history of pancreatic cancer-doctors can use special tools. Endoscopic ultrasound and MRI scans can catch tumors early in these groups. Programs like the one at Johns Hopkins have been doing this since 2010, and they’ve saved lives.
Still, most people don’t know they’re at risk. Only 12% of late-stage patients had genetic testing. Among those diagnosed early, 44% had already been tested because of family history. That gap is huge. If you have a parent, sibling, or child who had pancreatic cancer, ask your doctor about genetic counseling.
What Are the Latest Treatment Breakthroughs?
For decades, pancreatic cancer was seen as untreatable beyond surgery. But now, treatment is becoming more personalized and more effective.
Surgery is still the only way to potentially cure it. The Whipple procedure removes the head of the pancreas, part of the small intestine, gallbladder, and sometimes part of the stomach. For patients whose cancer hasn’t spread, this can lead to a 20-25% five-year survival rate. But not everyone is a candidate. Only about 15-20% of patients are diagnosed early enough for surgery.
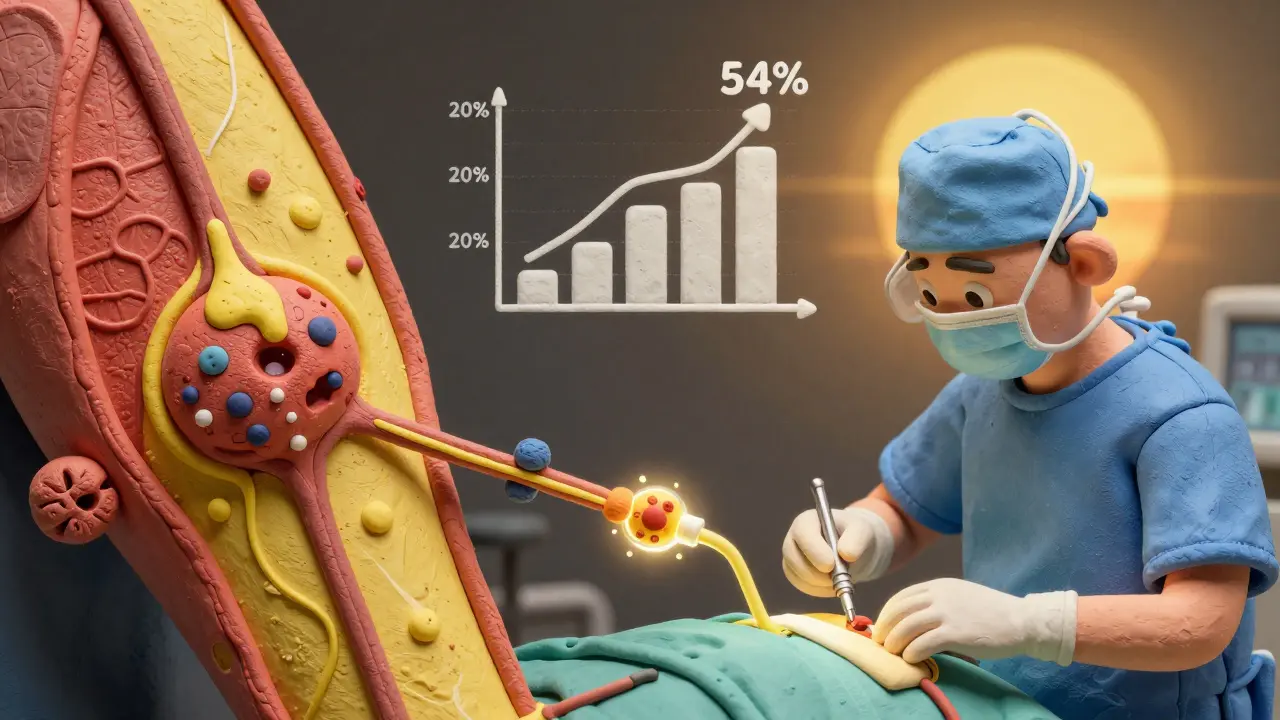
Chemotherapy before surgery (called neoadjuvant therapy) is changing that. Drugs like FOLFIRINOX-a mix of four chemotherapy agents-are shrinking tumors so that patients who once couldn’t have surgery now can. One 2021 trial showed a 58% response rate in borderline resectable tumors. That means more people get a shot at cure.
For advanced cancer, the game has changed. In 2022, a major trial showed that patients on modified FOLFIRINOX lived an average of 54.4 months-nearly 4.5 years-compared to just 20 months with older treatments. That’s not a cure, but it’s life-changing.
Targeted therapies are helping specific groups. If your tumor has a BRCA gene mutation, the drug olaparib can slow progression for over 7 months longer than placebo. If your cancer has a rare feature called MSI-H/dMMR (found in 3-4% of cases), pembrolizumab can trigger strong immune responses. These aren’t for everyone, but for those who qualify, they’re powerful.
What’s Coming Next: Blood Tests, AI, and Early Detection
The future of pancreatic cancer care isn’t just about better drugs-it’s about catching it sooner.
Tests like PancreaSeq, developed at Johns Hopkins, can detect early-stage cancer in high-risk people with 95% accuracy by analyzing DNA in pancreatic fluid. The DETECTA trial is testing a simple blood test that looks for tumor DNA and protein markers. Early results show 85% accuracy.
Artificial intelligence is stepping in too. Google Health’s LYNA algorithm can spot cancer cells on tissue slides with 99.3% accuracy-better than many human pathologists. And researchers are even studying gut bacteria. A 2023 study found that the microbiome in pancreatic cancer patients looks different from healthy people, and a stool test could identify the disease with 80% accuracy.
These aren’t just lab ideas. They’re moving fast into real-world use. The National Cancer Institute aims to cut pancreatic cancer deaths by 25% by 2030. That goal feels possible now, because the tools to get there are finally here.
What Should You Do If You’re Worried?
If you’re experiencing multiple unexplained symptoms-weight loss, new diabetes, jaundice, or persistent depression-don’t wait. Ask your doctor for a referral to a gastroenterologist. Request imaging if symptoms persist. If you have a family history of pancreatic, breast, ovarian, or colorectal cancer, get genetic counseling.
There’s no magic bullet, but awareness saves lives. Most people with early-stage pancreatic cancer have no symptoms at all. That’s why the focus now is on high-risk groups: people with new-onset diabetes after 50, those with inherited gene mutations, and families with multiple cases of cancer.
Progress is real. Survival rates are climbing. What used to be a death sentence is now, for some, a manageable condition. And for others, it’s becoming preventable-if we catch it early enough.
Can pancreatic cancer be cured?
Yes, but only if caught very early-before it spreads. Surgery to remove the tumor is the only cure, and it’s possible in about 15-20% of cases. For those patients, 20-25% survive five years or longer. For most, the goal is to extend life and improve quality with chemotherapy, targeted therapy, and clinical trials.
Is there a blood test for pancreatic cancer?
There’s no single blood test that works for everyone. CA 19-9 is used to monitor treatment in advanced cases, but it’s not reliable for early detection-it misses early tumors in up to 70% of cases. New tests are in development, like those that detect tumor DNA or protein patterns in blood. Some show over 85% accuracy in early trials, but none are standard yet.
What are the risk factors for pancreatic cancer?
Major risk factors include smoking (doubles the risk), long-term diabetes, chronic pancreatitis, obesity, and age (most cases occur after 65). Inherited gene mutations like BRCA1, BRCA2, Lynch syndrome, and familial atypical mole-malignant melanoma (FAMMM) also increase risk. A family history of pancreatic cancer raises your chance significantly.
Why is jaundice a key symptom?
Jaundice happens when a tumor in the head of the pancreas blocks the bile duct. This stops bile from reaching the intestines, causing bilirubin to build up in the blood. That leads to yellow skin, dark urine, and pale stools. It’s one of the clearest signs that something is wrong in the pancreas, especially if it appears without gallstones or liver disease.
Can lifestyle changes reduce the risk?
Yes. Quitting smoking is the most important step-it cuts your risk in half over time. Maintaining a healthy weight, eating a diet rich in vegetables and whole grains, and limiting red and processed meats also help. While you can’t change genetics or age, these choices lower your overall cancer risk, including pancreatic cancer.
What should I ask my doctor if I have new-onset diabetes?
Ask: "Could this be related to pancreatic cancer?" Especially if you’re over 50, have no family history of diabetes, and aren’t overweight. Request a CT scan or MRI of the abdomen if symptoms like weight loss or abdominal pain are present. Early detection is possible-if you push for it.

Glenda Marínez Granados
So let me get this straight... we're supposed to panic because we lost 5 pounds and got a little moody? 🤡 Next they'll tell me my cat staring at me is a sign of pancreatic cancer. I'm just here for the memes, not the medical horror show.
Yuri Hyuga
This is exactly the kind of life-saving information we need more of. 🌟 Awareness isn't just a buzzword-it's a lifeline. If just one person reads this and gets tested because of unexplained weight loss or new-onset diabetes, that's a victory. Keep sharing the facts. Knowledge is power, and power saves lives. You've done a tremendous service here.
MARILYN ONEILL
I read this and thought wow this is so basic. My cousin had this and she didn't even know. Like duh if you're losing weight and your eyes are yellow you should go to the doctor. Also why is everyone acting like this is new news? My grandma knew about jaundice in the 70s. People just don't listen.
Coral Bosley
I lost 18 pounds in 3 months last year. No diet. No exercise. Just... gone. And I was so depressed I couldn't get out of bed. My doctor said it was stress. I believed him. Now I'm terrified. What if I had waited another month? What if I'd just ignored it? I'm not even mad-I'm just hollow. I wish someone had told me sooner.
Steve Hesketh
Brothers and sisters, listen up! This isn't just science-it's survival. Every single one of you reading this? You could be someone's miracle. Maybe your mom. Maybe your dad. Maybe your best friend. Don't wait for the screaming. Listen for the whisper. Ask for the scan. Push for the test. Your courage today could be their tomorrow. You got this. I believe in you.
shubham rathee
I think the real issue is the pharmaceutical companies hiding the cure. Why else would they not have a blood test yet? And why is everyone so quiet about the link to 5G towers and glyphosate? I read a guy on YouTube who said he cured his pancreas with lemon water and quantum healing. He's alive. The system doesn't want you to know. I'm not paranoid. I'm prepared.
Kevin Narvaes
i mean like... its just cancer right? like we all gonna die anyway. why stress about one type? i had a friend who got diagnosed and he just chillaxed and ate tacos and lived 8 years. so maybe just live your best life and dont overthink it? 🤷♂️
Dee Monroe
I’ve been thinking about this a lot lately-not just medically, but existentially. The body whispers, yes, but so does time. And we’re so busy screaming into our phones that we forget to listen to the quiet signals. The pancreas doesn’t beg for attention-it just fades. And when it does, it takes with it the unspoken promises we made to ourselves: to eat better, to move more, to love deeper. Maybe this isn’t just about early detection. Maybe it’s about waking up before it’s too late to live.
Rod Wheatley
This is gold. Seriously. I work in primary care, and I’ve seen too many patients dismissed because 'it's just stress' or 'you're getting older.' Please, if you're over 50 and have two or more of these symptoms-don't take no for an answer. Demand an ultrasound. Insist on a CA 19-9. If your doctor won't help, go to urgent care or a GI specialist. Early detection isn't luck-it's persistence. You owe it to yourself.
Samuel Mendoza
Most of these symptoms are normal. People get tired. They lose weight. They get depressed. Stop fearmongering. If you're healthy, you're fine. If you're not, you'll know. Stop overtesting and overdiagnosing.
Sangeeta Isaac
so like i went to the doc last month cuz i was tired and my pee was dark and she gave me a vitamin b12 shot and told me to drink more water. now i'm wondering if i just missed my chance to catch cancer. 🤔 maybe i should've demanded a ct scan? idk. i'm just vibin'
Alex Carletti Gouvea
This is why America needs better healthcare. In my country, we don't wait for symptoms-we screen everyone. You think this is hard? Try living where your doctor doesn't even have a stethoscope. Stop complaining. Get tested. Or don't. But don't blame the system when you're too late.
Philip Williams
The data presented here is compelling and methodologically sound. The integration of AI diagnostics, particularly the LYNA algorithm, represents a paradigm shift in histopathological analysis. Furthermore, the longitudinal survival data from modified FOLFIRINOX trials demonstrates statistically significant improvement (p < 0.001). This is not anecdotal-it is evidence-based medicine at its most transformative.
Ben McKibbin
I lost my dad to this. He was 61. He had all the symptoms-weight loss, new diabetes, back pain-but he was too proud to go to the doctor. He thought it was just aging. I wish I’d pushed harder. I wish I’d known then what I know now. If you’re reading this and you have a loved one who’s stubborn? Don’t wait. Be the annoying one. Make the appointment. Sit in the waiting room with them. It might be the most important thing you ever do.
Melanie Pearson
The assertion that early detection is viable is a dangerous oversimplification. The false-positive rate of emerging biomarkers remains unacceptably high, and widespread screening would lead to unnecessary surgeries, psychological trauma, and healthcare inflation. The current focus on high-risk populations is prudent. To promote population-wide vigilance without validated tools is not awareness-it is alarmism.