Syphilis Oral Symptom Checker
This tool helps you identify potential oral syphilis symptoms and stages based on the information you provide. Remember: this is for informational purposes only. If you experience any of these symptoms, consult a healthcare professional immediately for proper diagnosis and treatment.
When you hear the word "syphilis," you probably picture a rash or genital sores. But the infection can also show up right in your mouth, and many people miss the warning signs until they’re serious. This guide walks you through how syphilis reaches the oral cavity, what the lesions look like at each disease stage, how dentists spot them, and what steps you can take to get back to a healthy mouth.
How syphilis reaches the mouth
Syphilis is caused by the spirochete Treponema pallidum a thin, corkscrew‑shaped bacterium that slips through mucous membranes. The organism can enter the body through any tiny break in the skin or mucosa - a kissing bite, oral sex, or a cut inside the cheek are all possible entry points. Once inside, it travels through the bloodstream and can settle in oral tissues, especially the soft palate, gums, and tongue.
Oral signs in primary syphilis
Primary syphilis typically appears about three weeks after exposure. Most people associate the primary sore with the genitals, but a primary syphilis the first stage of infection marked by a single, painless ulcer called a chancre can develop anywhere the bacteria entered - including the lips or inside the mouth.
- Location: usually on the inner lip, the tongue, or the soft palate.
- Appearance: a small, round, raised ulcer with a clean base; the edges may look slightly raised.
- Feel: completely painless, which often leads to it being ignored.
The chancre heals on its own in two to six weeks, but the bacteria remain in the body, ready to move to the next stage.
Oral signs in secondary syphilis
Secondary syphilis is the most contagious phase and shows up a few weeks after the primary chancre disappears. This stage brings a flood of mucous membrane lesions that are easy to spot if you know what to look for.
- "Mucous patches": flat, gray‑white plaques that may bleed if scraped. Common on the tongue, inner cheeks, and soft palate.
- "Condyloma lata": moist, wart‑like growths that prefer the genital area but can appear on the lips or perianal region.
- Generalised redness and swelling of the gums ("syphilitic gingivitis").
These lesions often come with a skin rash on the palms and soles, fever, and swollen lymph nodes. Because the mouth is highly visible, dental visits during this stage can lead to an early diagnosis.
Oral signs in tertiary syphilis
If untreated, about 15-30% of people progress to tertiary syphilis years later. Oral involvement at this stage is rare but serious.
- Gummatous ulcers: deep, painless cavities that can erode bone in the jaw.
- Destruction of the hard palate or alveolar bone, leading to loose teeth.
- Neurological involvement ("tabes dorsalis") can cause a loss of facial sensation, making oral injuries go unnoticed.
These problems can mimic other serious dental diseases, so a thorough medical history is crucial.

Diagnosis: What dentists look for
Dental professionals are trained to differentiate infectious lesions from common ulcers or irritations. When they see a suspicious mouth sore, they usually follow a step‑by‑step protocol:
- Take a detailed sexual and medical history (confidentially).
- Inspect the lesion’s size, shape, color, and pain level.
- Perform a rapid treponemal test on a swab or blood sample.
- Refer the patient to a primary‑care physician or an infectious‑disease specialist for confirmatory testing.
Early detection not only prevents mouth damage but also stops further spread of the infection.
Treatment and oral health recovery
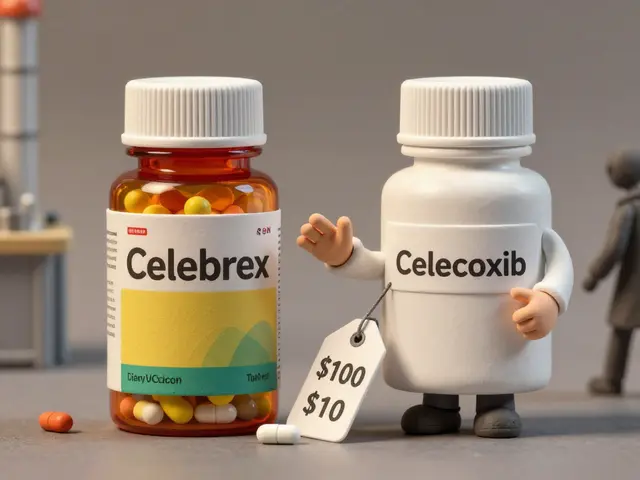
The gold‑standard cure for syphilis is a single dose of penicillin a beta‑lactam antibiotic that eradicates Treponema pallidum, administered intramuscularly. For patients allergic to penicillin, doxycycline is an alternative, though follow‑up testing is essential.
- Lesions usually begin to heal within a few days of treatment.
- Gingival inflammation subsides as the bacterial load drops.
- Regular dental cleanings after therapy help restore gum health and prevent secondary infections.
It’s important to complete the full antibiotic course and attend all follow‑up appointments. Even after the infection clears, some oral damage (like bone loss) may be permanent and require restorative dentistry.
Prevention and safe practices
Preventing oral syphilis is largely about reducing exposure to the bacterium:
- Use condoms or dental dams during oral sex.
- Get tested regularly if you have multiple partners - many clinics offer free rapid tests.
- Inform your dentist of any recent STI testing or diagnoses; they can monitor for related oral changes.
- Vaccination isn’t available for syphilis, but staying up‑to‑date on CDC the US Centers for Disease Control and Prevention, which publishes STI guidelines and WHO recommendations helps you follow the latest prevention advice.

Quick checklist: Spotting syphilis in your mouth
- Any painless ulcer on the inner lip, tongue, or palate lasting >2 weeks?
- Gray‑white patches that bleed when scraped?
- Unexplained gum redness or swelling?
- Joint appearance of a skin rash on palms/soles and oral lesions?
- Recent history of unprotected oral sex?
If you answer "yes" to one or more, schedule a dental exam and consider an STI test. Early treatment restores oral health fast and cuts transmission risk.
Understanding the link between syphilis oral health and overall wellbeing
Oral health isn’t isolated - it mirrors what’s happening in the rest of your body. Untreated syphilis can lead to systemic complications like heart disease, neurological damage, and pregnancy loss. By catching mouth signs early, you protect not just your teeth but your whole health.
Comparison of oral manifestations by syphilis stage
| Stage | Typical Lesion | Common Location | Duration (if untreated) |
|---|---|---|---|
| Primary | Chancre (painless ulcer) | Inner lip, tongue, soft palate | 2‑6 weeks (heals on its own) |
| Secondary | Mucous patches, condyloma lata, gingivitis | Tongue, cheeks, gums, soft palate | Weeks to months |
| Tertiary | Gummatous ulcers, bone destruction | Jawbone, hard palate, alveolar ridge | Years (may become permanent) |
Frequently Asked Questions
Can syphilis be spread through a simple kiss?
Transmission via a kiss is rare but possible if one person has an open mouth sore (like a chancre) and the other has a break in the oral lining.
Do oral syphilis lesions hurt?
Primary chancres are typically painless. Secondary lesions may be tender if they become inflamed or ulcerated, but many patients notice little pain.
How soon after treatment will my mouth feel normal?
Most oral lesions start to improve within a few days of a penicillin injection, and complete healing occurs within 2‑4 weeks, provided you follow up with dental care.
Is there a vaccine for syphilis?
No vaccine exists yet. Prevention relies on safe sexual practices, regular testing, and prompt treatment.
Should I tell my dentist if I’ve been diagnosed with syphilis?
Absolutely. Dentists need the information to monitor for oral manifestations and to protect staff with proper infection‑control measures.






Avril Harrison
In the UK we’ve actually seen a few cases where a painless ulcer on the palate turned out to be syphilis, and dentists were the first to spot it. It’s a good reminder that oral health isn’t just about cavities.
Sarah Hanson
The clinical manifestations described align with standard CDC guidelines; it is essential that practitioners maintain vigilance for painless chancre lesions. Prompt serologic testing definitively confirm the diagnosis, definatly.
Nhasala Joshi
💥🚨 The syphilitic spirochetes are nothing short of nano‑warriors, infiltrating mucosal barriers with quantum stealth; the epidemiological shadow‑network behind oral transmission is vastly under‑reported. 🧬🔬 Remember, every unexamined mouth could be a covert vector! 😱
Karla Johnson
When I first read about the oral manifestations of syphilis, I was struck by how easily they can be mistaken for common aphthous ulcers, especially in patients who doesn’t disclose their sexual history. The primary chancre, while painless, often goes unnoticed because it doesn’t cause discomfort, and many people simply think it’s a minor irritation. In the secondary stage, the mucous patches and condyloma lata can appear on the tongue, inner cheeks, and soft palate, creating a clinical picture that overlaps with candidiasis, lichen planus, or even leukoplakia. This overlap underscores the importance of a thorough differential diagnosis that includes a detailed sexual history, even though patients might be hesitant to share such information. Dentists, who see the oral cavity regularly, are uniquely positioned to catch these lesions early, which can dramatically reduce disease transmission and prevent progression to the destructive tertiary stage. The diagnostic protocol typically involves a visual inspection, followed by a rapid treponemal test on a swab or blood sample, and finally referral for confirmatory serology. Treatment with a single intramuscular dose of penicillin is remarkably effective, and lesions usually begin to resolve within days, though full mucosal healing may take weeks. Post‑treatment follow‑up is crucial, because serologic titers must be monitored to ensure eradication, and any persistent oral lesions warrant re‑evaluation for possible co‑infections. Moreover, practitioners should educate patients about oral hygiene practices that can support recovery, such as gentle brushing, antiseptic mouth rinses, and avoiding irritants like tobacco and alcohol. It’s also vital to counsel patients on safe sexual practices, including the use of dental dams during oral sex, to prevent reinfection. While no vaccine exists for syphilis, public health initiatives that promote regular STI screening have been shown to reduce incidence significantly. In addition, awareness campaigns that highlight the oral signs can empower individuals to seek care promptly, which is especially important in communities with limited access to healthcare. Finally, the psychological impact of an STI diagnosis should not be overlooked; providing compassionate counseling can help patients navigate the stigma and adhere to treatment plans. All these factors together illustrate how interdisciplinary collaboration between dentists, primary care physicians, and public health officials is essential for controlling the spread of syphilis and preserving oral health.
Linda A
In reflecting upon the cascade of clinical steps, one perceives a microcosm of broader human vulnerability; the mouth, a portal of expression, becomes a silent witness to unseen battles.
Joe Moore
Yo, they don't tell ya that the big pharma labs are cashing in on penicillin stock every time a syphilis case pops up – it's like a hidden profit engine behind every injection, man.
Ayla Stewart
I hear your point, but from a dental perspective the priority is still early detection and treatment to protect patients' health.
Stephanie Zaragoza
Indeed, the epidemiological data-when scrutinized-reveals patterns that are not merely coincidental; however, attributing causality to profit motives without robust evidence risks undermining public trust, which is, undeniably, a delicate balance.
James Mali
Honestly, the whole discussion feels like an overblown drama about a bug that can be killed with a single shot; maybe we should just focus on basic hygiene.
Janet Morales
That attitude ignores the lived reality of countless individuals who endure painful stigma; dismissing syphilis as mere drama does a disservice to those fighting an invisible battle.
Tracy O'Keeffe
Oi, mate, think again – treating syphilis like a simple cough is a naive oversimplification, and the cultural narrative around it is far richer than your lazy summary suggests, ya know?
Rajesh Singh
It is our ethical duty to confront the spread of syphilis head‑on, for turning a blind eye not only jeopardizes oral health but also erodes the moral fabric of our communities.
Albert Fernàndez Chacón
I totally agree, and I think supporting patients with clear information and compassionate care can make a real difference in outcomes.
Drew Waggoner
That’s exactly the approach we need.