Imagine your heart feels like it's tap-dancing in your chest and the medicine that was supposed to keep the beat—sotalol—just isn't doing the trick. Maybe the side effects are hitting too hard or your doc's worried about your kidneys. If this sounds familiar, you’re not alone. Atrial fibrillation can trip up even the most tried-and-true meds. Lately, more people are looking for alternatives that offer a better balance between results and side effect trade-offs. But which ones are best, and how do you pick between names like amiodarone and dofetilide—or the newer, flashier medications?
It gets complicated. Most folks want to avoid reading medical textbooks when all they want is a heart that behaves. The good news? There are options. And your choices don’t have to be educated guesses or shots in the dark. Let’s pull the curtain back on sotalol alternatives, talking side effects, lab stats, and what it’s really like day-to-day with these drugs.
When Sotalol Falls Short: Why Look for Alternatives?
Plenty of folks start with sotalol for atrial fibrillation because it checks a lot of boxes. It’s been around for ages, acts as both a beta-blocker and antiarrhythmic, and docs feel comfortable with its track record. But nobody mentions it's not always the smooth ride it promises. Some people get stuck with fatigue, dizziness, or even a strangely slow heartbeat. There’s also this gnawing worry about QT prolongation—which can turn into life-threatening rhythm problems of its own if you’re not careful.
Here’s a quick stat: around 20% of people on sotalol end up dropping the drug within the first year, according to a real-world heart clinic analysis in 2022. The two top reasons? Either the heart rhythm still goes haywire, or the side effects become unbearable. Those numbers make it clear: there’s demand for something safer, slicker, or just easier to live with.
What’s wild is that not all alternatives work the same way. Where sotalol blocks both beta-receptors and potassium channels, drugs like amiodarone and dofetilide are much more about taming the electrical system from different angles. Doctors weigh things like your kidney and liver health, other medications, and even your age or how easy it’ll be for you to get bloodwork. If you’re poking around for options, there’s a good spot to check out a wider list of sotalol alternatives, including what makes each one unique.
Sticking with sotalol because it’s familiar is like wearing shoes that give you blisters—sure, they fit, but there’s probably a better pair out there. Your heart deserves that upgrade.
Amiodarone: Built for Power, Not for Perfection
Ask any heart doctor their go-to for stubborn atrial fibrillation, and you’ll hear about amiodarone. It’s boldly effective: over 60% of patients maintain a normal rhythm after a year, beating out almost every other antiarrhythmic for this job. People who’ve been hospitalized for heart flutters swear by it, especially if nothing else seems to stick. The stats support it—one major U.S. dataset from 2023 showed amiodarone kept patients in normal rhythm twice as well as sotalol.
But this drug isn’t the ‘set it and forget it’ type. Amiodarone stays in your body for months, lingering long after you stop taking it. It means once you start, you may deal with its side effects for a while. And boy, are those side effects worth talking about. The big hitters are thyroid changes (since it’s packed with iodine), liver bumps, skin turning a bluish hue in certain spots if you’re out in the sun, and, rarely, lung scarring. The annual checkup laundry list for someone on amiodarone is serious—pulmonary tests, liver panels, eye exams, and thyroid checks. My neighbor, Jack, ended up having to memorize his lab draws better than his wi-fi password.
What’s neat is amiodarone is incredibly forgiving on the kidneys, so it’s often picked for people with less-than-stellar renal function. It also plays nice with heart failure, an area where lots of arrhythmia drugs can make things much worse. But be careful: it interacts with so many other meds, you almost need a spreadsheet. My wife Felicity once joked our fridge would need a second door, one just for her pill schedule if she was on amiodarone.
If power and staying in regular rhythm are your north star, amiodarone often comes out ahead. But be ready to monitor, and talk straight with your doctor about every new symptom—even the weird ones.
Dofetilide: Precision with a Side of Caution
Dofetilide is one of those drugs doctors silently cheer when it works well. It offers a much more targeted approach—zero effect on blood pressure, so it’s good if your numbers tend to dip. In studies (like the 2019 DIAMOND-CHF trial), it proved just as good, if not better, than sotalol when it came to keeping people out of atrial fibrillation. It’s the antiarrhythmic of choice for folks who also have congestive heart failure.
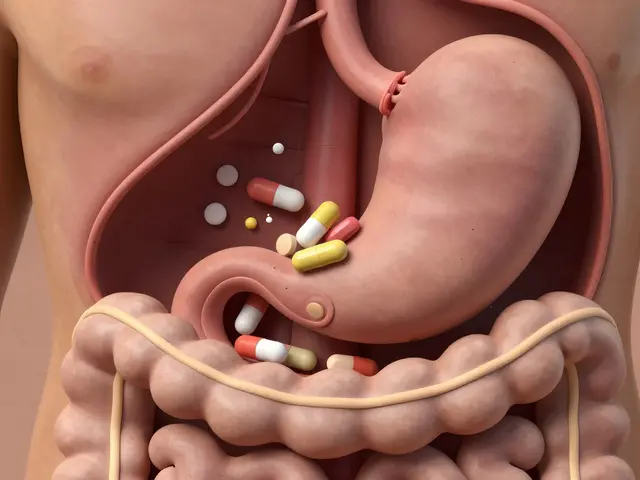
What’s the catch? Dofetilide is tricky to start. The first three days, you’re often monitored in the hospital—your heart gets watched, the nurses check your potassium and creatinine, and everyone keeps an eye on QT intervals, which can become dangerous if things get off balance. It’s a bit of an ordeal, but once you’re safely on it, you usually don’t need as much hand-holding as with amiodarone.
Other quirks? It’s cleared by the kidneys, so if your kidney numbers slide, your doc may say it’s a no-go. You can’t take it if you’re also on certain antibiotics, diuretics, or antifungals. The oddest thing might be that, for once, you don’t have to worry about liver problems—a nice change after scrolling through endless medication warnings.
Daily life on dofetilide is usually uneventful unless a side effect pops up. There may be a little dizziness, some headache, or unexplained tiredness. If you miss a dose, doctors get particular about what to do next, so always double-check rather than wing it. Felicity once said it’s like keeping up with a watering schedule for sensitive houseplants: regular, consistent, and don’t try to double up if you forget. That’s good advice.
When you want measured precision in keeping atrial fibrillation out of your life, and you don’t mind a brief hospital stay upfront, dofetilide might hit the sweet spot.
Novel Antiarrhythmics: What’s on the Horizon?
If you feel like you’ve heard the same handful of names since the 90s, there’s a reason. New antiarrhythmic drugs don’t flood the market often—safety testing takes years because heart rhythm problems turn critical fast. But in the last few years, researchers have gotten creative, and a few new contenders are making ripples.
Dronedarone is the one you’ll see most—designed to work like amiodarone but without the long-term fallout. Its liver and lung risks are way lower. But here’s the rub: it doesn’t stick quite as well in keeping atrial fibrillation at bay, with about 35-40% staying in rhythm after a year based on several big European studies. It’s also off-limits for people with serious heart failure; the risk for major problems actually goes up in that group.
Vernakalant is another one, but it’s only available in the U.S. as an IV drug—great for flipping someone out of atrial fibrillation quickly in the hospital but not something you’ll take at home.
There’s a buzz about upcoming medicines that can fine-tune their effect, shutting down arrhythmia but leaving healthy rhythm untouched. But they’re not in your pharmacy yet. What’s encouraging is that drug companies are investing more than ever—one report in 2024 showed a 20% year-over-year increase in antiarrhythmic research funding.
Here’s a look at how the main alternatives stack up statistically for keeping someone in normal rhythm after one year:
| Medication | % in Normal Rhythm (1 Year) | Major Side Effect Rate |
|---|---|---|
| Sotalol | 40-45% | 12% |
| Amiodarone | 60-65% | 19% |
| Dofetilide | 55% | 14% |
| Dronedarone | 35-40% | 10% |
No drug comes without trade-offs, but you can see why amiodarone’s name keeps coming up in tough cases. The end goal? Keep the heart calm—and keep you feeling like yourself.

Tips for Picking the Right Drug—and Talking with Your Doctor
Choosing which antiarrhythmic to try isn’t something to stumble into. You need a game plan so your heart (and your peace of mind) don’t get thrown around. Here’s how I’d approach it if I were in your shoes—or, honestly, how I did for my own family:
- sotalol alternatives all have different monitoring demands. Know how often you’ll need EKGs or blood tests—the less stressful, the better for most people.
- Think about your daily routine. Busy folks who travel for work may prefer medicines with fewer interactions and less strict dosing.
- If you have kidney or liver disease, make sure your doctor has every lab report handy. A single overlooked number can rule out an entire class of medications.
- Ask about what side effects usually show up early and which ones are slow creepers—some drugs, like amiodarone, go quiet for months before issues surface.
- If you notice new tiredness, coughing, vision changes, or rashes soon after starting a medicine, call right away. Don’t wait it out.
- Be honest if you struggle to take a medicine the same time every day. Some meds have very little wiggle room for missed or doubled doses.
The wildest part is how much heart rhythm medicine is trial and error. You may try one, step back, try another. Sometimes the first one becomes a winner. When things get tricky, be patient—stay plugged into your care team, and don’t settle for "just getting by." Your heart beats half a million times a week. Each one’s a vote for your health. You get a say in which medicine leads the charge.





Naomi Shimberg
While the allure of novel antiarrhythmic agents may appear compelling, one must consider the profound implications of long‑term organ toxicity that accompany agents such as amiodarone. The pharmacokinetic profile of amiodarone, with its extensive tissue accumulation, renders the drug a double‑edged sword: its efficacy in maintaining sinus rhythm is undeniable, yet the attendant risks of thyroid dysfunction, hepatic injury, and pulmonary fibrosis demand vigilant surveillance. Dofetilide, though praised for its renal clearance and precision, imposes a rigid initiation protocol that can burden patients with prolonged hospitalization and intensive electrolyte monitoring. Moreover, the necessity of frequent EKG assessments to preempt QT prolongation introduces an additional layer of complexity that may be untenable for individuals with limited access to care. The newer agents, including dronedarone, while ostensibly designed to mitigate the adverse effect spectrum, nonetheless suffer from reduced efficacy in patients with compromised ventricular function. It is also incumbent upon clinicians to recognize that the decision matrix extends beyond mere statistical outcomes; patient lifestyle, comorbidities, and personal preferences constitute critical variables. The presumption that a higher % in normal rhythm automatically translates to superior therapeutic value is simplistic, disregarding the nuanced trade‑offs each medication imposes. In practice, the selection of an antiarrhythmic must be individualized, balancing the probability of arrhythmia recurrence against the latent potential for organ toxicity. The dictum "first, do no harm" remains paramount, necessitating a cautious appraisal of long‑term sequelae. Accordingly, the decision to transition from sotalol should be predicated upon a comprehensive risk‑benefit analysis, not merely on singular efficacy metrics. Finally, the financial implications of ongoing laboratory and imaging studies associated with drugs such as amiodarone cannot be ignored, as they impose substantial economic strain on patients and healthcare systems alike. In summation, the clinician must navigate these intricacies with both scientific rigor and compassionate judgment, recognizing that the optimal therapeutic pathway is seldom linear.
kenny lastimosa
Choosing an antiarrhythmic is akin to navigating a philosophical labyrinth where each turn reveals the subtle interplay between the heart's rhythm and the body's equilibrium. The silent contract between patient and medication demands respect for the unseen consequences that emerge over time. One must weigh the promise of sinus stability against the quiet whisper of potential organ strain. In the grand tapestry of health, the pursuit of rhythm preservation should not eclipse the reverence for holistic wellbeing. The essence of this decision lies not in the loud proclamations of efficacy alone, but in the gentle acknowledgement of the body's intricate response to pharmacologic influence.
Heather ehlschide
When evaluating alternatives to sotalol, start by cataloguing your baseline labs-renal function, hepatic enzymes, and thyroid panels. Amiodarone requires quarterly thyroid and liver tests, whereas dofetilide mainly hinges on serum potassium and creatinine. If you have stable kidney function, dofetilide may spare you the extensive monitoring schedule of amiodarone. Conversely, in patients with compromised renal clearance, amiodarone’s minimal renal impact can be advantageous. Additionally, consider drug‑drug interactions; amiodarone has a notorious profile that can affect warfarin, statins, and many anti‑platelet agents. Dronedarone, though less toxic, should be avoided in heart‑failure patients due to increased mortality risk. Finally, discuss with your cardiologist the feasibility of initial inpatient monitoring for dofetilide, as this can affect convenience and insurance coverage.
Kajal Gupta
Hey folks, I totally get the hustle of trying to pick the right rhythm‑fixer without turning your life upside down. Amiodarone is like that heavyweight champ-big power, but you gotta watch for those sneaky side‑effects that pop up like surprise fireworks. Dofetilide, on the other hand, feels more like a precision laser-quiet and focused, just make sure your kidneys are in good shape and you’ve got the hospital stay covered. If you’re into a low‑maintenance vibe, dronedarone might be your jam, though it’s not the best pick if you’ve got serious heart failure. Bottom line: match the med’s personality to yours-whether you’re chill with regular labs or you need something that fits in a tight schedule. Stay safe and keep that ticker humming!
Zachary Blackwell
They don’t tell you that the pharma giants are hiding the real cure.
prithi mallick
I totally hear you, and it can feel like a maze when every option has a hidden trap. Remember, the heart is a living organ that responds uniquely to each med, so listening to your body is key. If you ever feel a strange cough or a shift in energy levels, it might be the early whisper of a side effect-dont ignore it. Also, keep a simple journal of symptoms; it helps you and your doc spot patterns faster. And yea, typos happen-just make sure your med list is clear, 'cause a little mix‑up can lead to big trouble.