Psoriasis isn’t just a rash. It’s a lifelong condition that changes how your body works - from your skin to your heart. If you’ve been told you have psoriasis, you’re not alone. Around 2-3% of people worldwide live with it, and for many, it’s more than flakes and red patches. It’s fatigue, joint pain, anxiety, and the constant worry that your skin might flare again. The good news? We know more now than ever about how to manage it - not just on the surface, but deep inside.
What Psoriasis Really Is
Psoriasis is an autoimmune disease. That means your immune system, which should protect you from germs, mistakenly attacks your own skin cells. Normally, skin cells take about 28 to 30 days to grow, die, and shed. In psoriasis, that process speeds up to just 3 to 4 days. The cells pile up before they can fall off, forming thick, scaly plaques - usually on elbows, knees, scalp, and lower back. It’s genetic. If someone in your family has it, your chances go up. Studies show a 60% to 90% heritability rate. But genes alone don’t cause it. Triggers like stress, infections (especially strep throat), cold weather, smoking, and certain medications can turn on the disease in people who carry the risk. There are different types. Most people (80-90%) have plaque psoriasis - the classic raised, red, scaly patches. Others get guttate (small drop-like spots), inverse (smooth, raw patches in skin folds), pustular (pus-filled bumps), or erythrodermic (a rare, full-body redness that can be life-threatening). Each type needs a different approach.Why Skin Care Isn’t Enough
Topical treatments - creams, ointments, lotions - are the first step. For mild cases, they work well. Common options include corticosteroids to reduce inflammation and calcipotriol (a vitamin D analog) to slow skin cell growth. Many doctors combine them into one product, like calcipotriol/betamethasone, to make it easier to use. But here’s the catch: topical treatments only go so deep. They don’t fix the immune system problem. And they’re hard to stick with. A Reddit survey of 247 people with psoriasis found that 67% struggled with consistency. Why? Messy applications, time, and fear of steroid side effects like thinning skin or stretch marks. Some areas are tricky. The face, genitals, and skin folds need gentler options. Strong steroids can damage thin skin. For the scalp, foam or solution forms work better than thick ointments. For nails, topical treatments often fail - and that’s when you know it’s time to think beyond the surface.When You Need Systemic Therapy
If your psoriasis covers more than 5% of your body, affects your nails or joints, or ruins your quality of life, you likely need systemic therapy. These treatments work inside your body to calm the immune system. Traditional systemics include:- Methotrexate: Taken weekly, it slows skin cell turnover and reduces inflammation. Side effects include nausea and liver stress - regular blood tests are required.
- Cyclosporine: Works fast, often used for sudden flare-ups or erythrodermic psoriasis. But it can harm kidneys, so it’s not for long-term use.
- Acitretin: An oral retinoid, helpful for pustular or erythrodermic types. Can cause dry skin, hair loss, and is unsafe during pregnancy.
The Biologic Revolution
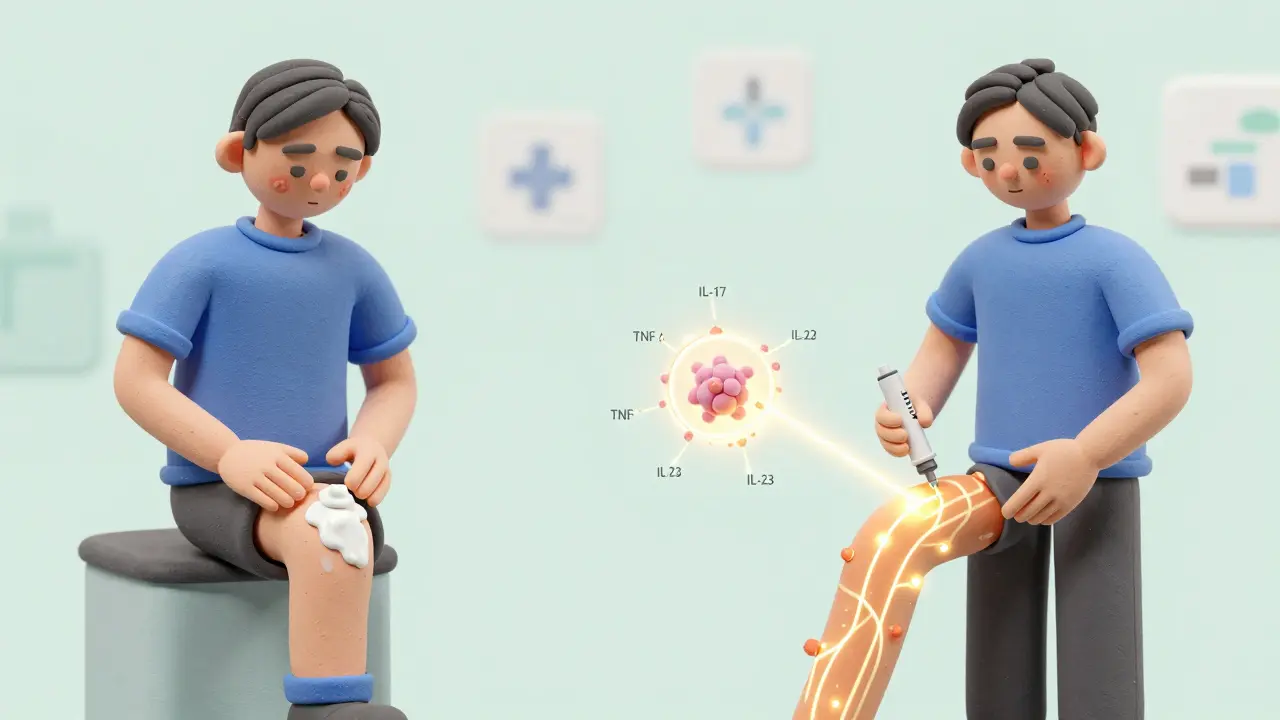
Biologics are the biggest leap in psoriasis treatment in decades. They’re made from living cells and target specific parts of the immune system. Instead of suppressing everything, they zero in on the culprits: TNF-alpha, IL-17, IL-23. Here’s how they break down:- TNF-alpha inhibitors (adalimumab, etanercept): First-generation biologics. Effective, but can increase infection risk.
- IL-17 inhibitors (secukinumab, ixekizumab): Fast-acting. Many patients see 90%+ skin clearance in 12 weeks.
- IL-23 inhibitors (guselkumab, tildrakizumab): Newer, longer-lasting. Some only need dosing every 8 to 12 weeks after initial doses.
The Hidden Costs - Physical and Financial
Psoriasis doesn’t just live on your skin. It’s linked to serious health problems.- Psoriatic arthritis: Affects up to 30% of people with psoriasis. Joint pain, stiffness, swelling - especially in fingers, toes, and spine. Early detection is key. If you have nail pitting or scalp psoriasis, get checked.
- Heart disease: People under 50 with psoriasis have a 58% higher risk of heart attack. The inflammation driving psoriasis also damages blood vessels.
- Metabolic syndrome: 40-50% of patients have high blood pressure, high cholesterol, or diabetes. This isn’t coincidence - it’s part of the disease.
- Depression and anxiety: 17-37% of patients struggle with mood disorders. That’s nearly 5 times higher than the general population.
Living With It: Daily Habits That Help
No treatment works well without daily care.- Moisturize daily: Use thick, petrolatum-based creams or ointments. Apply right after a shower while skin is damp. This traps water and reduces flaking.
- Use gentle cleansers: Avoid harsh soaps. Look for fragrance-free, non-detergent formulas. Lukewarm showers are better than hot ones.
- Track triggers: Keep a simple journal. Did your skin flare after stress? After drinking alcohol? After a cold? Patterns help you avoid flare-ups.
- Don’t scratch: It makes plaques worse. Keep nails short. Use cold compresses or anti-itch creams if needed.
- Quit smoking: Smoking doubles your risk of severe psoriasis and makes treatments less effective.
What’s Next in Treatment
The future is personalized. Researchers are moving beyond “one-size-fits-all.” New oral drugs like deucravacitinib (a TYK2 inhibitor) are already approved. Taken daily, it cleared 58% of patients’ skin by 16 weeks - comparable to injectables, but without needles. Oral RORγt inhibitors are in Phase 2 trials. They target the same pathway as biologics but are pills. If approved, they could replace injections for many. But there’s a problem: 75% of psoriasis research funding goes to biologics. That leaves room for innovation in oral and topical options - especially for people who can’t afford or tolerate injections.Where to Find Support
You don’t have to do this alone.- National Psoriasis Foundation: Offers free virtual support groups, educational webinars, and financial aid programs.
- MyPsoriasisTeam: A social app with over 175,000 users sharing tips, tracking symptoms, and connecting with others.
- PCDS patient leaflets: Updated in January 2025, these QR-coded guides explain treatments and self-care in plain language.
- Local dermatology clinics: Ask about patient navigation services - some help with insurance appeals and treatment access.
Frequently Asked Questions
Is psoriasis contagious?
No, psoriasis is not contagious. You cannot catch it from touching someone’s skin, sharing towels, or being near them. It’s an autoimmune condition, caused by your body’s own immune system going off track. There’s no virus, bacteria, or fungus involved.
Can psoriasis go away forever?
Currently, there’s no cure. But many people achieve long-term remission - months or even years without symptoms - with the right treatment. Some biologics keep skin clear for over a year between doses. The goal isn’t just control; it’s near-complete clearance and a normal life.
Do I need to see a dermatologist, or can my GP handle it?
Mild psoriasis can often be managed by a general practitioner. But if you have moderate to severe disease, joint pain, or if topical treatments aren’t working after 2-3 months, you need a dermatologist. They have access to advanced treatments like biologics and can screen for related conditions like psoriatic arthritis.
Why do some treatments stop working over time?
Your immune system can develop resistance to some treatments, especially biologics. This is called tachyphylaxis. It’s not failure - it’s biology. When that happens, switching to a different class of drug (like going from a TNF inhibitor to an IL-23 inhibitor) often brings results back. Your doctor will adjust your plan based on how your body responds.
Can diet or supplements cure psoriasis?
No diet or supplement can cure psoriasis. But some people notice fewer flares when they reduce alcohol, lose weight, or avoid processed foods. Omega-3s and vitamin D may help a little, but they’re not replacements for medical treatment. Always talk to your doctor before starting any supplement - some can interfere with your medications.
How do I know if my psoriasis is getting worse?
Watch for signs: new plaques appearing, existing ones getting larger or thicker, skin cracking or bleeding, joint pain, or feeling more tired than usual. If your DLQI score (a quality-of-life questionnaire) goes up, or if you’re avoiding social situations because of your skin, it’s time to talk to your doctor. Don’t wait until it’s unbearable.
What to Do Next
If you’re just starting out:- Get a proper diagnosis. Not all scaly skin is psoriasis.
- Ask about screening for psoriatic arthritis and heart risks.
- Start a skin diary - note flares, triggers, and what helps.
- Find a dermatologist who listens. Treatment is personal.
- Explore support groups. You’re not alone.
- Don’t stop because of cost or side effects - talk to your doctor about alternatives.
- Ask if you’re on track for PASI 90 or DLQI ≤4.
- Review your medications annually. New options appear every year.
- Check your blood pressure and cholesterol. These matter as much as your skin.





Oladeji Omobolaji
Been dealing with this since I was 16. Got mine on my elbows and scalp. Topicals? Meh. They work for a bit, then you’re back to scratching like a dog with fleas. Biologics changed my life - no more hiding my arms in summer. Cost is insane, but my insurance covered it after I fought for six months. Worth it.
Also, quit smoking cold turkey. My skin cleared up before the meds even kicked in.
Janet King
Psoriasis is an autoimmune disorder characterized by accelerated keratinocyte proliferation and chronic inflammation mediated by T cells and cytokines. Topical therapies such as corticosteroids and vitamin D analogs are first-line for mild disease. Systemic agents including methotrexate and cyclosporine are indicated for moderate to severe cases. Biologics targeting interleukin-17 and interleukin-23 pathways have demonstrated superior efficacy in achieving PASI 90 response rates. Patient adherence remains a critical factor in long-term outcomes.
Andrew Smirnykh
I’ve lived in three countries and seen how differently psoriasis is treated. In the US, it’s all about biologics. In Nigeria, where I’m from, most people use herbal pastes or just endure it. I wish more doctors here knew about the link to heart disease - my uncle had a stroke at 48 and no one connected it to his scalp psoriasis.
Maybe we need global guidelines. Not everyone can afford a $5,000 shot.
Kerry Evans
People act like psoriasis is just a skin thing. It’s not. It’s a failure of personal responsibility. You smoke? You’re dumb. You’re overweight? You’re lazy. You skip moisturizer? You’re unhygienic. This isn’t a mystery - it’s a mirror. Your body is screaming at you to take care of yourself. Stop blaming the medicine. Start blaming your choices.
And yes, I’ve had it since I was 19. I’m 52 now. Clear skin. No biologics. Just discipline.
Susannah Green
Okay, real talk: moisturizing after the shower? YES. But use the thick, greasy ones - Vaseline, CeraVe, Eucerin. Not that watery lotion you buy at the drugstore. It’s useless. I use a 16oz tub of plain petrolatum. Costs $8. Lasts six months.
Also - stop using hot water. It’s like sandpaper on your skin. Lukewarm. Five minutes max. Pat dry. Don’t rub. Then slather.
And yes, I’m a nurse. I’ve seen this a thousand times.
Anna Pryde-Smith
MY SKIN IS ON FIRE AGAIN. I JUST GOT BACK FROM THE DERM. THEY WANT TO PUT ME ON A BIOLIC. I’M SCARED. I’M 28. I DON’T WANT TO BE ON INJECTIONS FOREVER. I JUST WANT TO WEAR A TANK TOP WITHOUT FEELING LIKE A MONSTER. WHY DOES THIS HAVE TO BE SO HARD? I’M SO TIRED.
Anyone else feel like your skin is the only thing people see? Like your personality doesn’t exist?
Vanessa Barber
Wait, so biologics are the new miracle cure? Interesting. But didn’t we say the same thing about phototherapy in 2008? And then it turned out half the people got no benefit and the other half got skin cancer? I’m not saying don’t try it. I’m just saying… maybe don’t treat it like a religion.
dana torgersen
you know... i think psoriasis is not just a disease... it's a message... from the universe... or maybe your subconscious... your skin is reflecting your inner chaos... like... if you're holding onto anger... or fear... or unprocessed trauma... it comes out as scales...
i started journaling and doing breathwork... and my plaques... they... faded... not because of meds... but because i finally let go...
psoriasis... is just your body screaming... 'i'm not ok'...
and yeah... i know... it sounds like woo... but... have you ever really listened... to your skin?
Dawson Taylor
Effective management requires a systems approach. Topical therapy addresses surface symptoms. Systemic and biologic interventions target immune dysregulation. Lifestyle modifications reduce triggers. Screening for comorbidities improves long-term outcomes. Adherence is the most significant variable in treatment success. The goal is not cure, but function. Quality of life is the only true metric.