Medication Adherence vs. Compliance: It’s Not Just Words
You’ve been prescribed a pill. Every day. For months. Maybe years. You mean to take it. You even set reminders. But some days, you skip it. Maybe because it makes you feel sick. Maybe because it’s expensive. Or maybe you just forgot. Now your doctor says you’re non-compliant. But that’s not the whole story.
Here’s the truth: the word "compliance" is outdated. And using it can hurt your care. The healthcare world has moved on. Today, the focus is on medication adherence-and that shift isn’t just about language. It’s about saving lives.
What Does "Compliance" Really Mean?
"Compliance" used to be the go-to term. If you took your pills exactly when told, you were compliant. If you didn’t, you were labeled non-compliant-like a child who didn’t clean their room. It was a one-way street: doctor gives orders, patient follows.
This approach assumes patients have no say. No worries. No life. No side effects. No bills. But that’s not real life. A 72-year-old with diabetes might skip insulin because the co-pay doubled last month. A young mother might forget her blood pressure pill because her toddler woke up screaming at 3 a.m. Calling that "non-compliance" ignores the human side of medicine.
Compliance is still used in rare cases-like directly observed therapy for tuberculosis, where a nurse watches you swallow every pill. But for chronic conditions like high blood pressure, cholesterol, or depression? It’s the wrong tool for the job.
What Is Medication Adherence-and Why It’s Better
Medication adherence is different. It’s not about obedience. It’s about partnership.
The American Pharmacists Association defines adherence as "the extent to which a patient’s behavior matches agreed-upon recommendations." Notice the word "agreed-upon." That’s key. Adherence means you and your provider talked. You shared your fears, your schedule, your money problems. Together, you made a plan that actually fits your life.
And it’s measurable. The American Medical Association says you’re adherent if you take at least 80% of your prescribed doses over time. Not 100%. Not perfect. Just 80%. That’s realistic. That’s human.
Adherence looks at the whole picture: Did you start the medicine? Did you keep taking it? Did you stop because of side effects? Did you run out and couldn’t refill? All of that matters.
Why the Shift from Compliance to Adherence Happened
The change didn’t happen overnight. It started in the 1990s when doctors realized something shocking: about half of all patients stop taking their meds within the first year. Not because they’re lazy. Because the system wasn’t working for them.
Studies in the Journal of Clinical Pharmacy and Therapeutics and the Annals of Internal Medicine showed that blaming patients didn’t improve outcomes. In fact, it made things worse. Patients felt judged. They stopped talking. They stopped showing up.
Then came patient-centered care. The idea that you’re not a passive recipient-you’re a partner. Your voice matters. Your life matters. Your reasons matter.
By the early 2000s, major medical journals stopped using "compliance." The FDA and European Medicines Agency now require adherence data in clinical trials. The Centers for Medicare & Medicaid Services started tying hospital payments to adherence rates in 2024. This isn’t a trend. It’s a transformation.

How Adherence Leads to Better Outcomes
Here’s what happens when you focus on adherence, not compliance:
- Patients are 2.57 times more likely to stick with their meds when they feel heard (NCPA, 2022)
- Health systems using adherence programs see 37.6% higher adherence rates (NCPA, 2022)
- Patients on adherence-focused plans have 20-50% higher treatment success rates (AHRQ, 2022)
- Adherence programs reduce avoidable hospital stays by 22-34% (McKinsey, 2024)
One Kaiser Permanente study used a smart pill dispenser called Hero Health. It tracked when pills were taken and sent alerts. Missed doses dropped by 42%. Why? Because it didn’t shame people. It helped them.
Another study with Dose Packer’s tracking system improved medication possession ratios by nearly 29% across 12,000 patients. That’s not magic. That’s listening.
What Gets in the Way of Adherence?
People don’t miss pills because they’re careless. They miss them because of real, everyday barriers:
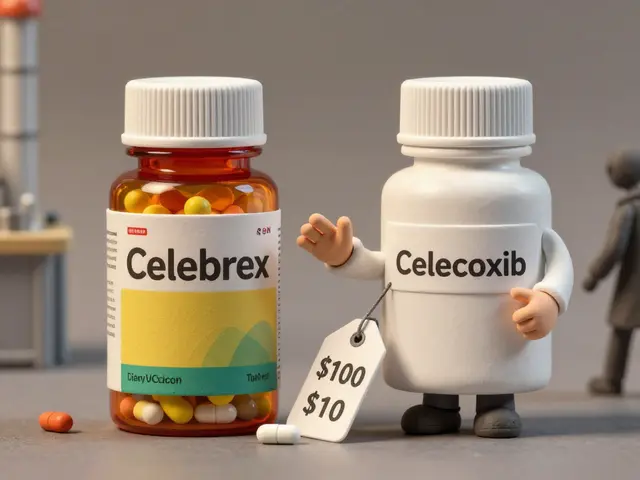
- Cost: A statin that costs £80 a month? Many skip doses to afford food.
- Side effects: Nausea, dizziness, fatigue-these are real, and they scare people off.
- Complex regimens: Ten pills a day? That’s hard to remember.
- Lack of understanding: "Why do I need this if I feel fine?"
- Cultural beliefs: Some people distrust pills. Others believe in natural remedies.
- Forgetfulness: Life gets busy. Especially if you’re juggling jobs, kids, or caregiving.
Compliance ignores all this. Adherence asks: "What’s stopping you? How can we fix it?"
How Providers Are Actually Helping Patients Adhere
Good providers don’t just hand out prescriptions. They have conversations.
They use tools like:
- Motivational interviewing: Asking open questions like, "What’s your biggest concern about this medicine?"
- Shared decision-making: Offering options. "We could switch to a once-daily version, or try a generic. Which feels more doable?"
- Personalized education: Not just handing out pamphlets. Showing you how to fit your pills into your morning coffee routine.
- Technology: Apps that send reminders, smart pillboxes that track opens, and EHR alerts that flag when refills are late.
Providers now need 8-12 hours of special training to do this well. It takes time. But it works. And it’s now billable. The AMA introduced new CPT codes (99487-99489) in 2025 specifically for adherence counseling. That means doctors get paid to listen.

The Future Is Personalized, Not Prescriptive
What’s next? AI.
Google Health’s 2024 study used machine learning to predict who’s likely to miss doses-not by looking at medical history, but by analyzing 27 factors: income, zip code, phone usage, appointment attendance, even social media patterns. The algorithm was 83.7% accurate.
That doesn’t mean robots are replacing doctors. It means systems can flag: "This patient hasn’t refilled in 45 days. They live near a food bank. They’ve missed two appointments. Let’s call them before they end up in the ER."
The World Health Organization projects that if we fully embrace adherence-focused care, we could prevent 850,000 premature deaths in low- and middle-income countries by 2030. That’s not a guess. That’s data.
What You Can Do Right Now
If you’re on long-term meds, here’s how to take charge:
- Ask questions: "Why am I taking this? What happens if I skip it? Are there cheaper options?"
- Speak up about side effects: Don’t just stop. Say, "This makes me feel awful. Can we adjust?"
- Use tools: A pill organizer, phone alarms, or apps like Medisafe or MyTherapy.
- Bring your meds to appointments: Show your provider exactly what you’re taking. You’d be surprised how often people mix up pills.
- Ask for help: Pharmacists are trained in adherence. Ask them to review your meds. Most pharmacies offer this for free.
You’re not failing if you struggle. The system failed you if no one asked why.
Why This Matters for Everyone
This isn’t just about pills. It’s about dignity. It’s about being treated like a person, not a problem to fix.
When you’re asked, "What’s getting in your way?" instead of "Why aren’t you following orders?"-you feel seen. And when you feel seen, you’re more likely to stick with your treatment.
Adherence isn’t about perfection. It’s about progress. It’s about collaboration. It’s about recognizing that healing isn’t a checklist. It’s a journey-and you’re not walking it alone.
Is medication adherence the same as compliance?
No. Compliance means following orders without question. Adherence means working together with your provider to find a plan that fits your life. Adherence considers your reasons, your barriers, and your choices. Compliance blames you. Adherence helps you.
What percentage of patients are considered adherent?
According to the American Medical Association, a patient is considered adherent if they take at least 80% of their prescribed doses over time. In reality, only about 50% of patients with chronic conditions meet this standard. That’s why adherence programs are so critical.
Why do people stop taking their medications?
There are many reasons. Cost is the biggest one-many skip doses because pills are too expensive. Side effects, forgetfulness, complex regimens, lack of understanding, and cultural beliefs also play a big role. Most people don’t stop because they’re lazy. They stop because the system doesn’t support them.
Can technology help with medication adherence?
Yes. Smart pill dispensers like Hero Health and tracking apps like Dose Packer have reduced missed doses by 40% or more in real-world studies. These tools don’t punish you-they remind you, track your progress, and alert your care team if you’re struggling. They’re part of a supportive system, not a surveillance tool.
What should I do if I can’t afford my medication?
Don’t skip doses or stop without talking to your provider. Ask your pharmacist about generic versions, patient assistance programs, or mail-order options. Many drug companies offer discounts. Your doctor can also switch you to a lower-cost alternative. You deserve care that fits your budget.
Is adherence only important for chronic conditions?
It’s most critical for chronic conditions like high blood pressure, diabetes, or depression-where missing doses over time leads to serious complications. But even for short-term treatments like antibiotics, adherence matters. Stopping early can lead to resistant infections. The principle is the same: take it as agreed, not just as convenient.
Why did healthcare stop using the word "compliance"?
Because it was harmful. Studies showed blaming patients for not following orders made them feel ashamed and less likely to return for care. The shift to "adherence" in the early 2000s reflected a move toward patient-centered care. It acknowledges that patients are partners, not passive subjects. Major organizations like the FDA, WHO, and AMA now require adherence-focused language.
Can my doctor tell if I’m not taking my meds?
They can suspect it. Blood tests, refill records, or missed appointments can hint at non-adherence. But they won’t know the real reason unless you tell them. That’s why open conversations matter. If you’re struggling, say so. Your doctor’s job isn’t to judge-it’s to help you succeed.






Claire Wiltshire
This is such an important shift in healthcare language. 'Compliance' implies obedience, but 'adherence' recognizes that people are complex humans with real barriers. The 80% threshold is brilliant-it’s not about perfection, it’s about partnership. I’ve seen patients disengage when labeled 'non-compliant,' but when providers ask 'What’s getting in the way?'-that’s when real change happens.
Pharmacists are the unsung heroes here. Free med reviews? Yes, please. We need more of that.
Mike Rose
idk why people make such a big deal about this. just take your pills. if you can’t afford them, get a job. problem solved.
Russ Kelemen
This isn’t just about meds. It’s about dignity. The moment we stop seeing people as problems to fix and start seeing them as partners in healing-that’s when medicine becomes humane. I’ve had patients cry because no one ever asked why they stopped their pills. They didn’t need a lecture. They needed someone to sit with them. And now, doctors get paid to do that? Long overdue.
Adherence isn’t a metric. It’s a mindset. And it’s the only way we’ll ever fix the broken parts of this system.
Darren Gormley
lol 'adherence' is just woke corporate jargon for 'we’re too scared to call people out for being lazy'. 80%? That’s just letting people off the hook. If you’re supposed to take a pill every day and you miss 20%? You’re not 'adherent'-you’re irresponsible. And now we’re paying doctors to coddle people instead of holding them accountable? 🤡
Diksha Srivastava
I’m from India and this hits so hard. My grandma skips her BP meds because she thinks 'if I feel fine, I don’t need it'. But when we talk about it like a team effort-'what if we try a cheaper pill?' or 'can we set a reminder with your favorite song?'-she starts taking it. It’s not about force. It’s about love. 🙏
Sidhanth SY
Honestly, the word 'compliance' always felt off to me. Like I was a robot being programmed. Adherence? That’s real. I’ve got a 3-year-old, a night shift, and a $200 co-pay. I don’t skip meds because I’m lazy-I skip because I’m exhausted. If my doctor had asked me 'what’s stopping you?' instead of giving me side-eye? I’d still be on track.
Adarsh Uttral
this is good but like… who has time for all this? my phone dies, my app dont work, i forget. its not that i dont care, its just life is chaos. maybe we need simpler tools, not more talking.
April Allen
The paradigm shift from compliance to adherence aligns with the biopsychosocial model of care, which acknowledges the interplay between biological, psychological, and sociocultural determinants of health behavior. The 80% adherence threshold is clinically validated and statistically significant in reducing morbidity and mortality in chronic disease management, particularly in hypertension and type 2 diabetes. The introduction of CPT codes 99487–99489 represents a structural reimbursement innovation that incentivizes behavioral health integration. This is not semantics-it’s systems-level reform.
owori patrick
In Nigeria, we have people who skip meds because the pharmacy is 3 hours away. Or because the price jumped 300% last month. Or because the doctor never explained why it matters. We don’t need more labels. We need more transport, more generics, more time with pharmacists. Adherence isn’t a buzzword here-it’s survival.
Sheila Garfield
I used to think people were just forgetful. Then my sister got diagnosed with depression and started skipping her meds because they made her feel numb. She didn’t tell anyone. I didn’t know until she almost ended up in the ER. It’s not about discipline. It’s about connection. If someone’s not taking their meds, ask them why. Not with judgment. Just… ask.
Shawn Peck
THIS IS THE MOST IMPORTANT THING YOU’LL READ THIS YEAR. PEOPLE ARE DYING BECAUSE DOCTORS ARE TOO LAZY TO LISTEN. I’VE SEEN IT. MY DAD DIED BECAUSE THEY CALLED HIM 'NON-COMPLIANT' WHEN HE COULDN’T AFFORD HIS HEART MEDS. NOW THEY WANT TO PAY DOCTORS TO TALK? IT’S ABOUT TIME. SHAME ON EVERYONE WHO SAID IT WASN’T A BIG DEAL.
Blair Kelly
The fact that we need a whole article to explain that calling people 'non-compliant' is dehumanizing is a national disgrace. This isn’t medical jargon-it’s moral clarity. The AMA finally caught up. The FDA didn’t wait. The WHO is saving lives with this. And yet some of you still think it’s just semantics? You’re not just wrong. You’re dangerous.
Sazzy De
i used to be the one skipping pills. then my pharmacist just asked me if i was scared of them. i cried. we switched to a liquid form. now i take them with my coffee. simple. no shame. just help.
Sarah Blevins
The literature consistently demonstrates that adherence-based interventions yield statistically significant improvements in medication possession ratios (MPR) and clinical outcomes. However, the operationalization of 'agreed-upon recommendations' remains inconsistently documented across primary care settings. Without standardized documentation protocols, the transition from compliance to adherence risks becoming performative rather than substantive.
Russ Kelemen
I read the comment from the Nigerian guy and the Indian mom. They’re not talking about jargon. They’re talking about survival. And the people saying 'just take your pills'? They’ve never had to choose between medicine and rent. Or medicine and their kid’s school lunch. This isn’t about discipline. It’s about justice.